Keratoconus: A Cornea Condition
Today I thought it would be a great idea to discuss a specific corneal condition that not only prevents a patient from having refractive surgery, like LASIK, but can also result in the inability to see clearly, sometimes even in glasses or regular contact lenses. This condition, called Keratoconus (pronounced ker-UH-toe-KOH-nus), is a corneal condition, meaning it affects the outermost part of the eye. Keratoconus occurs when the cornea slowly becomes thinner in certain areas, which then causes the cornea to bulge into a cone-like shape, which in turn distorts the person’s vision, causing significant blurred vision, shadowing, and can leave a person unable to fully enjoy their lives. I know, this sounds like a lot to digest and understand! So, let’s break this condition down further, looking at some of the causes, the symptoms, and the treatments that are currently available for patients, including patients that come through the doors of CArrot LASIK and Eye Center.
Is it Genetic: How can Keratoconus Occur?
Keratoconus, like many other conditions that affect the human body, is still being researched by medical professionals to be able to fully understand how and why it happens. As of today, medical professionals are still not sure as to why this condition occurs, although according to the Mayo Clinic, certain genetic conditions, such as Ehlers-Danlos Syndrome and Marfan Syndrome can predispose a person to having the condition, as well as having a close family member, such as a parent with the condition (Mayo Clinic, 2023). In fact, a recent study published in the European Journal of Human Genetics, was able to illustrate that there is a shared genetic component and etiology between the Ehlers-Danlos Syndromes (EDS) and Keratoconus, with many of their study participants having both of the genetic conditions (Fransen et al., 2021). In a very broad sense, bothe Ketatoconus and EDS are conditions in which collagen within the body is affected, whether that be just on the eye, or throughout the entire body. As someone with a subtype of EDS, I could spend the next several paragraphs, or pages, going into detail about this study and other important connections between Keratoconus and EDS, but alas, I will save that for another day! What is important to understand, is that although it appears there is a genetic component with Keratoconus, at this time, there still needs to be more research conducted to fully understand the condition. However, some other factors can contribute to a person developing Keratoconus, including excessive eye rubbing, and being having asthma or hay fever. Okay, now that we know a little bit about how a person can develop Keratoconus, let’s take a further look into what the condition actually is.
As I stated previously, Keratoconus occurs when the cornea becomes thin in some spots, which then causes the cornea to bulge, and results in the patient developing an irregular form of astigmatism. I am sure that many of you have heard of astigmatism, which is a condition that occurs when there are imperfections on the cornea, which affects the way it is curved, and in turn affects the way light is refracted into the eye. As Dr. Hammond likes to put it, “Astigmatism is the difference between the highest point on your cornea, and the lowest point.”. When a person has astigmatism, light is refracted into the eye in a distorted way, which can lead to the patient perceiving “shadowing” in their vision, and in cases of high amounts of irregular astigmatism, it can even make people feel as though they are experiencing double vision. In most cases, astigmatism can be corrected with glasses or soft contact lenses, and there are now many soft contact lenses on the market to help correct astigmatism. However, in the case of Keratoconus, the amount of irregular astigmatism present can become exceedingly hard to correct with glasses, or even soft contact lenses. We will get into the treatments that do work for correcting irregular astigmatism in a moment, but another important factor of Keratoconus that can affect a patient, is scarring on the cornea. This can occur for several reasons, but specifically in Keratoconus, swelling inside of the cornea can occur when a specific layer, called the Descemet’s Membrane starts to break down, and this can lead to fluid entering into the cornea, ultimately creating scarring on the cornea that can sometimes not be fully reversed. Along with irregular astigmatism, scarring on the cornea can lead to even further distorted vision, and can lead to an even lower quality of life for the patient. Now that I have probably worried you with all of this information, let’s talk about what can be done to help those with this condition.
Treatments for Keratoconus: Glasses, Contact Lenses, and Surgery
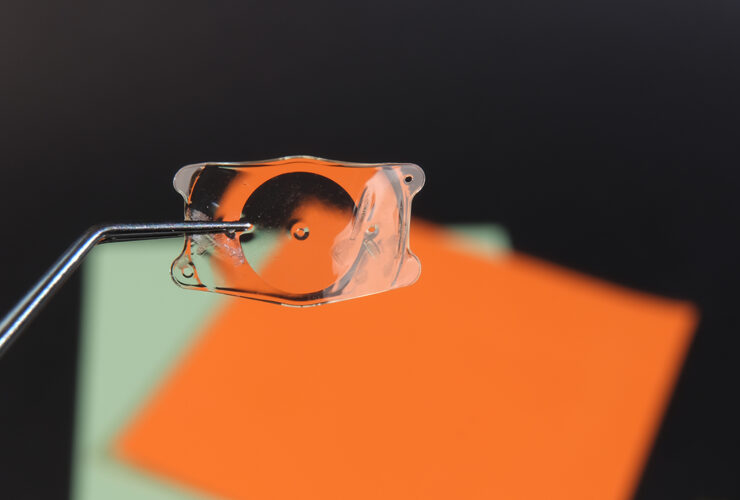
I am sure that it may seem like Keratoconus is a difficult condition to live with, and while it most certainly is, there is definitely hope for patients with the condition. Depending on when the patient receives their diagnosis, they may be able to have their vision corrected well with glasses and soft contact lenses. That being said, as the condition progresses, glasses and traditional soft contact lenses may not be able to fully correct the patient’s irregular astigmatism, in which case, they may have to switch to using scleral contact lenses. This is a special type of rigid contact lens that is made specifically for the patient’s eye, and it is much larger than a soft contact lens, as it not only covers the iris, the colored part of the eye, but also goes onto the sclera, the white part of the eye. When the patient puts the lens on their eye, they have to ensure they have the lens filled with a special saline solution, as the eyes must stay hydrated throughout the day, and this solution also helps with the clarity of the lens. Scleral lenses are amazing pieces of medical equipment, and with further advances in technology, optometrists, and some ophthalmologists, are able to make exact molds of the patient’s eye to ensure their scleral lens fits them perfectly. And unlike their soft counterpart, scleral lenses can last a patient up to a year, if not longer, when properly cared for.
If a patient has been diagnosed later in life, or if their condition has progressed, they may be able to undergo a procedure called Corneal Cross-Linking, which is a procedure that seeks to help improve the stability of the cornea through using Riboflavin, a protein that can help strengthen collagen on the cornea. This procedure is less invasive than others, however, if a patient’s Keratoconus is very advanced, they may not qualify for this procedure, and may have to undergo a corneal transplant. As with other transplants that take place throughout the body, a cornea transplant involves removing unhealthy corneal tissue, and replacing it with a donor’s. This procedure can be successful in some cases, however, there are many patients that may have to undergo several transplants, and may still not have clear or “usable” vision. I believe it is important to understand that while some cases of Keratoconus are quite severe, and a person may require all of the above treatments to help preserve their vision, it is best to look at the condition as on a spectrum, with there being very severe cases, but also mild cases.
Could You Have Keratoconus?
While Keratoconus is still considered a rare condition, with advances in medical technology over the past several decades, those living with the condition have been able to achieve a better quality of life with the help of procedures like corneal transplants, and devices such as scleral contact lenses. Although it is possible that you, or someone you know, may have Keratoconus, the signs and symptoms of the condition will normally present themselves in a person’s third decade of life, if not earlier. So, if you are reading this, and you have gained wisdom beyond your third decade of life, it is likely that you will not develop Keratoconus, or you may have a very mild case of the condition. All of that being said, it is imperative that you receive your annual eye exam, especially if you are having changes in your vision. While symptoms such as blurred, doubled, or shadowed vision can be indicative of having astigmatism, whether it be regular or irregular, can also be an indication of other vision changes, so please see your eye care professional as soon as you can, or at least on a yearly basis!
Does Carrot LASIK and Eye Center treat Keratoconus?
Dr. Herion and Dr. Hammond, while both very knowledgeable in Keratoconus and other corneal conditions, and are able to prescribe glasses and soft contact lenses to help with those conditions, they do not perform corneal cross-linking, corneal transplants, or fit patients for scleral lenses. However, because both doctors have been in this field for many years, they have great relationships with many corneal specialists and optometrists across the valley, and across the country, that are able to assist with more advanced corneal treatments and procedures. At Carrot, we want to ensure we are offering the best care possible to our patients, and while sometimes we cannot assist in all cases, we will make sure we are doing everything in our power to connect our patients with a top-notch medical team that can help with all of their needs. So please feel free to give our office a call with any concerns you may have, and we look forward to being able to help you with your vision needs!